Shin Splints / Medial Tibial Stress Syndrome
- Edel Kieran

- Mar 26, 2020
- 5 min read
What are shin splints?
Shin splint is a common overuse injury. In running sports (including multi-directional field sports) shin splints have been identified as the most common overuse musculoskeletal injury. Overuse injuries happen when repetitive small traumas to the bone exceeds the bone’s healing potential.
Shin splints is a common and vague term used to describe shin pain. The American Medical Association defines shin splints as “pain and discomfort in the leg from repetitive running on hard surfaces or forcible, excessive use of the foot flexors”. The clinical term for shin splints is "medial tibial stress syndrome".
Generally, shin splints refers to a stress reaction in the tibia from overuse.

What do shin splits feel like?
Usually, shin splints have a very gradual onset, there is no specific event that causes pain.
At first, the patient only feels a small amount of pain at the beginning of the workout / run. Oftentimes, the pain will disappear during the workout but may return soon after you stop.
Your pain will be made worse by weight – bearing activities (running / jumping). As this injury worsens, the pain will remain during exercise and you will often have pain for hours or days after your last workout.
Shin splints will often feel worse in the morning because the muscles / tendons tighten up overnight. A person suffering from shin splints will feel a sharp pain when they try to dorsiflex the foot and extend the toes.
If you are still suffering from pain a week after your last workout or if you have an obvious limp from pain, a therapist might query a stress fracture.

Who is at risk of developing shin splints?
Shin splints are most common in sporting populations, particularly in those sports involving running and jumping.
Individuals who are poorly conditioned are at a higher risk of developing shin splints.
It has been seen that young people are more susceptible than adults to bone stress injuries – between 40 – 50 % of all bone related stress injuries reported, are in athletes younger than 20 years old.
Cross country running and gymnastics have the highest incidences with girls having almost twice the risk as boys.
Girls with a delayed age of menarche (Menarche defines the onset of menstruation / age of your first period), a family history of osteoporosis or who are participating in high – impact activity have the highest risk.
Women who have a history of disordered eating, amenorrhea (lost their period for a length of time) and a low body mass index are also more at risk than those who have not.

Are there other risk factors for developing shin splints?
There are many factors that play into the development of shin splints.
Drastic increase in training load / intensity put a person at risk of developing shin splints. This increase can be increased distance, duration or speed. A change in your training surface is also a risk factor. (Changing from grass to road).
Muscular imbalance and inflexibility (particularly in the gastrocnemius, soleus and plantaris) are associated with shin splints. If you have muscle weakness in the gastrocnemius, soleus and plantaris, they are more prone to fatigue which will lead to changed running mechanics. These changes will them cause strain on the tibia.

The same rule applies for overall strength and flexibility, you need to use all your muscles to run / train. If these muscles are not strong enough, they will fatigue quicker and that will lead to a change in your running mechanics. From this, inadequate strength and flexibility are risk factors.
Nutrition plays a huge part in bone health. Calcium and vitamin D levels are the main nutritional factors that influence bone health.
Unhealthy sleep habits and psychological stress may also affect bone health.
How are shin splints treated?
Treatment for shin splints is generally conservative and no specific treatment has been shown to be more effective than other.
Generally, the first step in treatment is to modify your training. This can be a complete rest at first, in order to reduce the symptoms followed by a graded return to training. (Duration and intensity). Controlling your training surface is also an important consideration in the treatment of shin splints. You should start on a softer flatter surface and incorporate harder and more uneven surfaces as your rehabilitation progresses.
Along with graded return to training, you should implement a progressive rehabilitation programme. This rehab programme should aim to strengthen lower leg musculature and mobilise the ankle and foot. It is also advised that this programme addresses overall strength, particularly of the stabilising muscles in the hip and core. By strengthening these muscles and mobilising these joints, you aim to correct your running gait and increase your body’s ability to resist fatigue.
Proprioceptive (balance) training is also a key component of a shin rehabilitation programme. This trains your body to react to changes in underfoot surfaces without compromising running style / gait.
As we have previously mentioned, nutrition plays a big role in bone health. Optimising calcium and vitamin D intake is a good treatment and prevention measure to take.
It is important that people partaking in regular training, in particular those who would like to increase their training volume/ intensity are educated regarding proper diet, the importance of managing their load and the role that strength training plays in increasing training load.
Time to return to sport depends on injury location and severity.
Does my sport influence the location / severity of my injury?
Your specific sport may influence the location of your injury.
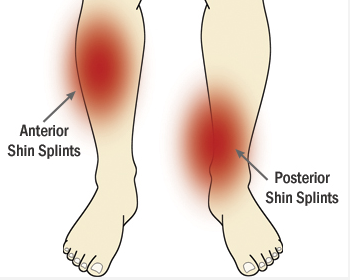
Injuries to the front, middle third of the shin are more common in jumping athletes. Most long distance runners have pain behind their shin, in the middle section. The lower third of the shin is injured more often in sprinters or in those who compete in sports with sprinting activity. The top third of the shin is commonly involved in pre – teen athletes.
With regard to severity, the key to ensuring that your injury does not become more severe is early detection and intervention. As we already mentioned, injury severity will affect your time to return to play.
What is the difference between shin splints and a tibial stress fracture?
As we have already mentioned, shin splints, known clinically as medial tibial stress syndrome. This means that most people presenting with shin splints have got a stress reaction on their tibia from overuse.
The most common complication of shin splints is a stress fracture. A stress fracture is an incomplete crack in the bone, also caused by overuse (normally).

The main differences between a stress fracture and shin splints is the pain associated with a stress fracture is specific and can be pin pointed and a definite point of pain. Generally, a person who has sustained a stress fracture with have pain on impact (even low impact) even after a period of rest. Additionally, stress fractures will often feel better in the morning as the bone has been rested all night.
Stress fractures have been shown to have long – term implications on bone health so modifiable risk factors should be addressed. This also highlights the importance of addressing shin splints early on, when they are easily managed.
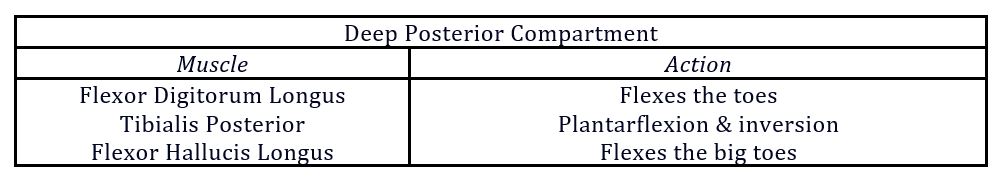
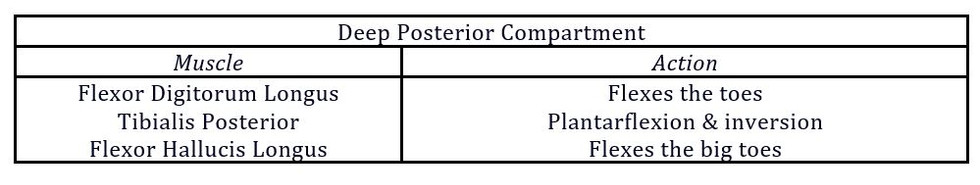
Anatomy of the Lower Leg:
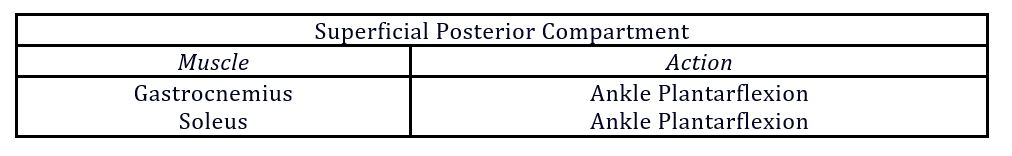
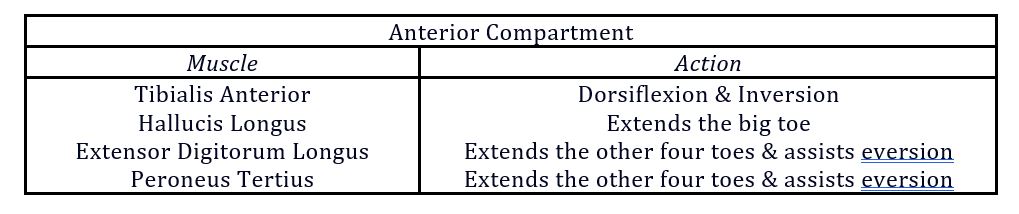
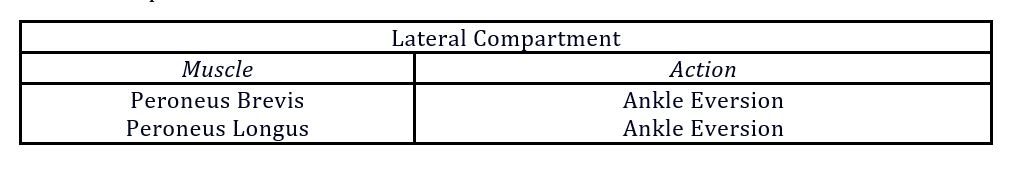
There are four main compartment in the lower leg:

















Comments